Michael Kirby AC CMG
BA LLM BEc (Sydney), DLit (hc) (Newcastle), LLD (hc) (Sydney), LLD (hc) (Macquarie), LLD (hc) (National Law School, University of India)
Justice of the High Court of Australia
Edition: AHRLJ Volume 4 No 2 2004
Pages: 163 - 180
Citation: (2004) 2 AHRLJ 163-180
Download article in PDF
One-time member of the World Health Organisation Global Commission on AIDS; member of the UNAIDS Reference Panel on HIV/AIDS and Human Rights. This paper is an expanded version of a paper delivered on 22 July 2004 as a 'University Lecture' at the University of Pretoria, where the author was a Yale Fellow of the Centre for the Study of AIDS and the Centre for Human Rights. These are the author's personal views.
Summary
From the outset, HIV/AIDS posed challenges that made traditional public health approaches, such as quarantine, inappropriate. The author realised early on in the epidemic that law had a role to play in curbing the spread of HIV, but that the temptation to adopt 'highly inefficient laws' had to be resisted. The first AIDS paradox arose when it became clear that the disease could best be curbed by respecting the rights of those infected with HIV, rather than by imposing restrictions on such persons, as traditional public health approaches or popular outcries for punishment demanded. This was so because only behaviour change could curb the spread of HIV, and a human rights-based approach was regarded as the most feasible way to ensure the knowledge of and means to effect behaviour change. The author identifies a second AIDS paradox, which accompanies the greater availability of antiretroviral treatment (ARV). Seeing the solution in greater access to ARV, he argues that consideration must be given to whether past strategies of testing and counselling should be amended to 'scale up' testing and, consequently, access to ARVs. Advocating a more flexible approach, the author poses the question whether a human rights-based approach should not be replaced by a serostatus-based approach.
1. Introduction
From the start, HIV/AIDS has not been like any other epidemic. The numbers of people infected were immediately far too numerous to warrant the traditional approach of quarantine. Furthermore, the long period of latency of the virus and the limited modes of transmission made such an approach disproportionate. The absence of a rapid cure and the failure to develop speedily a safe and effective vaccine has meant that HIV/AIDS is not susceptible to the usual medical or public health responses, used in the past in challenges of this kind. Moreover, the principal modes of transmission — penetrative sexual activity and injecting drug use (commonly involving stigmatised groups in the community: sex workers, men who have sex with men, and drug users), together with high initial levels of mortality and widespread community fear have made HIV/AIDS a most troublesome problem.
Faced with challenges of this kind, the natural human reaction is flight or fight. Unfortunately, flight, in the form of denial and neglect, has all too often been the response to HIV/AIDS. Particularly is this so in the developing world, and especially in South Africa where a state of denial appears to have paralysed many of those who should have been giving leadership. [1] In other parts of the developing world, denial took different forms. Often it has involved immobilisation of thinking and action on the part of leaders and officials, with a consequent unchecked rise in sero-conversions as more and more people became infected with HIV.
In sub-Saharan Africa, as in most parts of the developing world, HIV/AIDS has, from the start, followed the dominant pattern of typical transmission. Whereas in most developed countries the primary burden of HIV initially fell upon that cohort of the population involving men who have sex with men (primarily homosexuals), together with some injecting drug users, in Africa the pattern has been principally one of transmission through sexual contact between persons of the opposite sex, together with subsequent mother to child transmission to neonates and, in some cases, through breastfeeding. The result has been that in countries following this primary pattern (including South Africa), HIV/AIDS has leapt beyond small minority groups in the community. It has entered the cohort of the population comprising the overwhelming majority of the community. It has reached a level in terms of numbers and distribution [2] that, without radical interventions, will mean increased and ongoing dangers to the entire population — or at least a large proportion of those in the ages most vital to the economy, being the ages of work, sexual activity and child bearing.
I have been a witness to the epidemic of HIV/AIDS, virtually from the beginning. In Australia, the heaviest toll fell (and still falls) on the homosexual community. Because of my own sexuality, by the early 1980s, in Sydney, I became aware of the report of a strange new condition that, in large numbers, was striking gay men in Australia, the United States and elsewhere. In 1981, reports circulated in the gay media suggesting that a new condition resulting in swollen lymph nodes was caused by the use of 'poppers', pharmaceutical amyl nitrate originally intended for emergency relief of angina pectoris. This drug had come into recreational use in the 1960s in gay venues, often in conjunction with sex on premises. The initial reports led to publicity urging the curtailment of 'poppers' as hazardous to health. The sudden appearance of an increase in a previously rare condition of Kaposi's sarcoma amongst gay men who had used 'poppers' led to the understandable but erroneous belief that coincidence was explained by causation. [3] HIV/AIDS was not to prove so simple.
In the early days, theories abounded as to the cause and origin of the curious debilitating condition that was striking large numbers of otherwise healthy gay men. However, eventually it became clear that a new and dangerous epidemic was underway. Dr Peter Piot and his colleagues described the disease in Central and East Africa, [4] just three years after its first description in the United States. [5] These reports proved a grim herald for what was to follow.
Working in Congo (Zaire) as an epidemiologist, at the time of the early detection of the new 'slim' disease, was a young Jewish American medical scientist, Jonathan Mann. He later described how, during a visit to that country of the Director-General of the World Health Organisation (WHO), Dr Hafden Mahler, in the midst of an African thunderstorm, he explained to the world's top health bureaucrat the new medical condition and the challenges that it presented. Soon afterwards, Jonathan Mann was summoned to the WHO headquarters in Geneva. He was given a desk and a secretary but little else. Thus began the global response to AIDS.
Not long after his appointment, Jonathan Mann came to Australia. I met him at one of the first national conferences in my country concerned with the impact of the epidemic in Australia and its region. I was immediately struck by the high sense of dedication and commitment of Dr Mann. Most surprising of all was that he was speaking in a language that I understood: a language of human rights and individual protection. His was not the traditional language of the public health official. After I had published an essay on the subject of the legal responses to HIV, [6] some of my judicial colleagues at the time, in the Court of Appeal, expressed dismay that a judge was venturing into the forbidden territory of an epidemic connected with prostitutes, homosexuals, injecting drug users, sex venues, anal intercourse and other previously unmentionable topics. However, sitting by the bed of friends who had become infected with HIV, watching their struggle and believing that the law could play an affirmative role, I continued my involvement. For me, it was an ethical issue. People were dying. There were no drugs. There was no vaccine. Unusually, therefore, as Dr Mann taught, law had a positive role to play.
2. The first AIDS paradox
It must have seemed unusual to Jonathan Mann that a lawyer, and a judge, would be interested in the issues of HIV as I was. Soon after his visit to Australia, I was invited to become a member of the first Global Commission on AIDS. This was a supervisory body established by WHO to work in relation to the Global Programme on AIDS of which Jonathan Mann was the Director.
The Commission was chaired by the distinguished Swedish scientist, Professor Lars Kallings. It gathered participants from many parts of the world, with different expertise but a common commitment. Two of the scientific members of the Commission were Dr Luc Montagnier and Dr Robert Gallo, subsequently credited with the co-discovery of the virus (HIV) responsible for the breakdown in the body's immune system, resulting in AIDS. One of the most influential members of the Commission was Dr June Osborn, then professor of Public Health of the University of Michigan. From the start, Professor Osborn insisted that WHO, in all of its interventions on HIV/AIDS, should rest its strategies on the best available empirical data. AIDS was such an emotional, frightening and stigma-laden condition that nothing else would suffice. In the place of ignorance, superstition, moralising and fear would be substituted good science, empirical data and a sound knowledge of the epidemic and its modes of transmission.
This was the first real blow for respect for human dignity in the global struggle against HIV/AIDS. WHO would insist, from the outset, upon an empirical approach. It would oppose the extreme and disproportionate reactions of those who demanded quarantine or other protections excessive to the condition and irrelevant to the modes by which HIV was transmitted from one person to another.
Of course, from the earliest stages — and especially once the virus was described and tests were developed to the antibodies produced by the virus — demands were made for mandatory testing and for the introduction of laws that would strike down hard on the people who were thought to be responsible for spreading the virus. It was at this stage that I described two phenomena that were quickly to become features of the early global struggle against AIDS.
The first was the danger of a virus of a different kind, namely the virus of highly inefficient laws (HIL). [7] This was not a novel or unexpected response to an epidemic of such proportions. It had happened before in history. [8] But in the early days of AIDS, the pressure on legislators and governments to produce a legal response — any response — was enormous. That pressure presented the risk of making victims of everyone. [9] Effective and efficient laws, well targeted and proportionate, would be required. But the over-reach of law was a danger in epidemics. Together with many others, I lifted my voice in warning.
The second proposition that was expressed at this time was that AIDS was riddled with paradoxes. [10] The first and central paradox of HIV/AIDS, in the first decade after it manifested itself, was the one that became best known and best understood. According to this AIDS paradox, the most effective means of preventing the spread of the virus, at that stage, was protection of the human rights of the people most at risk of acquiring the virus. This was a paradox because it was contrary to intuitive responses to the spread of a dangerous virus in society. Instinctively, in such a case, citizen and public health experts thought in terms of the public health paradigm. Citizens, moreover, thought of punishment. Their minds were in tune with the moralising and stigmatising response that those who had and spread the virus were unclean, immoral and dangerous to the community — people who needed to be controlled, checked and sanctioned. The instinctive reaction of many people was to punish, to impose mandatory testing on large segments of the population and to denounce those considered responsible.
The difficulty with this approach was that HIV was unlike other conditions. During the long period of latency, people who had acquired the virus could continue performing their social and employment functions fully and without risk to others in most aspects of life. Because there was no specific treatment or vaccine, the only effective means of ensuring against infection by HIV was behaviour modification. Therapies could provide support and palliative assistance. But they could not rid the body of HIV as it could be relieved of tuberculosis and other infectious conditions.
Even if everyone in the community could be tested, at great expense, there were no desert islands and insufficient barbed wire to isolate those who came up positive. Behaviour modification thus, possibly for the first time, became the major focus of the strategy of the Global Programme on AIDS and the WHO Global Commission on AIDS. Instead of urging moralising, stigmatisation, punishment and quarantine, the approach of WHO embraced the 'AIDS paradox'. The best way to promote behaviour modification, essential to prevent the spread of HIV, was to ensure that knowledge about the existence, modes of transmission and means of prevention of infection was given to all those at risk of acquiring it in circumstances that they would trust, believe and follow up.
Thus was established the rights-based approach in the struggle against HIV/AIDS. In an article, [11] Dr Mann declared that '[h]ealth and human rights are complementary approaches to the central problem of advancing human well-being'.
In Australia, as a result of a rare co-operation between political leaders in government and opposition and in consequence of well-informed and enlightened leadership in politics and administration, the rights-based approach was observed, virtually from the start. [12] In Australia, radical measures were taken in pursuance of the initial AIDS paradox:
• A massive public information campaign on television and in other media was undertaken to alert the entire Australian community of the existence, dangers, modes of transmission and methods of protection in respect of HIV.
• A specific national structure, NACAIDS (the National Committee on HIV and AIDS) was quickly put in place to mobilise an ongoing national strategy and to devise particular policies, to support relevant interest groups and to promote research, science and information campaigns.
• All Australian health ministers, in an astonishing and courageous decision, agreed to a national needle and syringe exchange programme. This was the first formal, national recognition of the reality of illicit drug use in Australia. Implicitly, it involved a departure from the 'zero tolerance' approaches of the 'war on drugs'. It embraced harm minimisation. It did so on the footing that this was the most sensible policy to follow to arrest in the spread of HIV/AIDS. It became possible for injecting drug users to deliver used syringes to many pharmacies and other publicised outlets, with no questions asked, in exchange for sterile equipment so as to reduce the risk of infection by this route.
• Even in prisons, where multiple use of injecting drug equipment was one possible risk factor, enlightened prison administrators, whilst not supplying sterile injecting equipment in breach of prison regulations and safety, ensured that bleaching solutions were left available for use for sterilisation purposes by those in the prison who had gained access to such equipment.
• School education courses were introduced to inform students in most schools of the dangers of HIV and the modes of avoiding transmission, including the use of condoms.
• Dispensers for anonymous condom sales were introduced in many public places to permit acquisition of protectives, and to overcome the embarrassment or fear involved in purchasing them from pharmacies and stores.
• The remaining laws that were still in force in Australia for the criminalisation of adult, consensual homosexual conduct in private were repealed. The last such repeal followed federal legislation, [13] enacted by the Australian parliament following a ruling by the United Nations (UN) Human Rights Committee that the Tasmanian laws criminalising adult homosexual conduct [14] were contrary to Australia's obligations under the International Covenant on Civil and Political Rights (CCPR). [15]
• In many parts of Australia, the laws on prostitution have been reformed in order to reduce the risk of an underground culture out of contact with health messages and the empowerment necessary for self-protection amongst sex-workers. [16]
• To the anti-discrimination laws that were already enacted, provision was made in a number of states permitting remedies to persons who suffered discrimination on the ground of a relevant health status, including that of being HIV positive. [17]
In consequence of these radical measures, largely supported at the time by both major political groupings in Australia, the incidence of HIV infections throughout the nation dropped quite rapidly. The following graph illustrates the reported incidence of HIV in Australia from the beginning of the epidemic, taken at 1980, until the year 2000. [18]
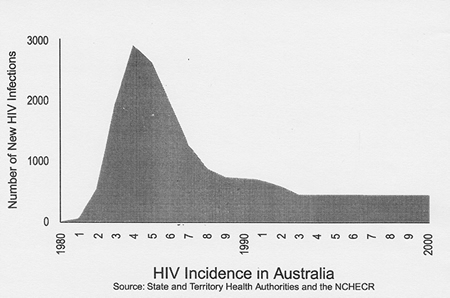
Appropriate credit must be given to the political leaders, their advisers and health officials who played a part in reducing the toll of HIV in Australia. Credit must also be given to NACAIDS and to organisations within the gay community who, at the start, were in the front line. In the past two years, for the first time, there has been an increase in the number of HIV sero-conversions in Australia as in other developed countries. This is a serious development. It appears to be related to fatigue in the gay community and the diminished power of the messages of self-protection after 20 years of relative success.
The availability of anti-retroviral treatment (ARVs) under the Australian Pharmaceutical Benefits Scheme for people in Australia living with HIV and AIDS has also had a consequence that individuals are less willing to treat HIV, as it still is, as a most serious risk to individual health, well-being and life. We still do not know how to rid the body of a person infected with HIV/AIDS of all traces of the virus. In this respect, HIV remains incurable. Those who are infected remain capable of infecting others. However, in developed countries, such as Australia (and particularly where they have effective national health systems), HIV is no longer the automatic death sentence that it was at the beginning of the epidemic. People living with HIV can ordinarily continue to live an economically productive life marked by human dignity.
By virtue of the early interventions, political leadership and sound policies in accordance with the first AIDS paradox, the rate of Australian infections never reached a plateau where it could take off and penetrate the entire community. In short, HIV was contained. Sadly, in Africa, there have been few cases of similar leadership. The lessons of the first AIDS paradox were not fully accepted in Africa. And even where they were, all too often they were corrupted by notions of moralising and stigmatising this human illness. Moreover, the funds were not available to provide access to ARVs. Even where they were, rapid steps have not been taken to make these life-enhancing and life-saving drugs available to the general population. This, therefore, brings me to the second AIDS paradox as it affects the situation in Africa at this time.
3. The second AIDS paradox
Come forward 20 years from the first rumours of the condition that turned into AIDS. Sadly, the fears of a major assault upon the health of people in all parts of the world have been fulfilled. HIV/AIDS, despite the enormous efforts of WHO and UNAIDS, which was established to co-ordinate UN's strategies in this area, has continued to expand. Indeed, at the XV International Conference on HIV/AIDS held in Bangkok in July 2004, the view was widely expressed that the pandemic of AIDS is now 'out of control'. [19] As if to symbolise the seriousness of the global predicament, the Secretary-General of the UN, Mr Kofi Annan, attended the biennial conference for the first time. He urged, not just for Africa, but for the world: [20]
We need leaders everywhere to demonstrate that speaking up about AIDS is a point of pride, not a source of shame. There must be no more sticking heads in the sand, no more embarrassment, no more hiding behind a veil of apathy.
The Bangkok conference demonstrated the impact of the 'culture wars' upon the controversies over HIV/AIDS, as on so much else in the world today. One of the liveliest debates in Bangkok concerned a shift towards abstinence as a prevention campaign, both in the United States and in some countries of the developing world. The President of Uganda, Mr Yoweri Museveni, told the Bangkok conference that the first line of defence against HIV/AIDS infection in Uganda was 'abstinence and faithfulness'. He declared that the use of condoms was 'an improvisation — not a solution'. [21] In this respect, his statement reflected the current policy of the United States government which has stepped away from the 'rights-based approach' (CNN — condoms, negotiations and [sterile] needles) anchored in virology instead of morality.
The so-called 'ABC' approach (A for Abstinence, B for Being Faithful and C for Condoms) has resulted in a substantial part of the large and generous funding offered and promised by the United States government being devoted to strategies of abstinence and faithfulness (strict monogamy and no sex before marriage). The cost effectiveness of such abstinence strategies has been questioned, although no one doubts that reduction in the number of sexual partners significantly reduces the risks of HIV infection. Total abstinence from sexual activity would self-evidently remove one of the main risk factors of infection, so long as it lasted. The question presented by the ABC strategy involves one of emphasis and ideology. To some extent, at least, the strategy responds to the moralising attitudes of religious and other groups who have been concerned from the first that the 'rights-based' strategy in respect of HIV/AIDS has undermined true morality, promoted promiscuity, condoned drug use and contributed to individual and community moral decay. [22]
For present purposes, these controversies can be placed on one side. They are important, but they are not the most important of the challenges to the 'rights-based approach'. This approach includes an insistence upon the right of individuals, who are adults acting with consent, to decide for themselves about their sexual behaviour in private, so long as it does not involve risk of harm to others. The real challenge to the 'rights-based approach' comes from a different quarter. It is the result of a realisation that not enough is being done to ensure the provision to millions of HIV infected people in the developing world of the ARVs that, in developed countries, are largely taken for granted in the medical management of the condition of HIV/AIDS.
Upon his election as Director-General of WHO, Dr Lee Yong-wook (Republic of Korea) declared that the current mortality from AIDS of approximately three million persons each year (mostly in the developing world and substantially in Africa) was totally unacceptable. If the enormity of this level of death and suffering is considered even for a moment, the conclusion of Dr Lee is plainly correct. Among the most fundamental of the human rights guaranteed by international human rights law is the right to life [23] and the right to access to health care. [24]
These fundamental rights are recognised in the International Guidelines produced by the Second International Consultation on HIV/AIDS and Human Rights, jointly organised by the UN Office of the High Commissioner for Human Rights and UNAIDS. [25] I chaired the consultation that produced those guidelines. They grew, in turn, out of an earlier (1989) consultation. They called on the member states of the UN to adopt a number of strategies, including legal strategies, to ensure a co-ordinated, participatory, transparent and accountable approach to HIV/AIDS, compatible with human rights and fundamental freedoms, in order to respond effectively to the epidemic.
Guideline 6 of the International Guidelines, as adopted in 1996, concerned the right of access to health care. As first drafted, the Guideline was qualified and cautious: [26]
Guideline 6: Regulation of goods, services and information
States should enact legislation to provide for the regulation of HIV-related goods, services and information, so as to ensure widespread availability of qualitative prevention measures and services, adequate HIV prevention and care information and safe and effective medication at an affordable price.
The original text of Guideline 6, as so accepted, reflected a number of considerations. These were the state of the pharmaceutical developments of therapies and vaccines in 1996; the state of the intellectual property regimes' national, regional and international, then in place; and the feasibility of securing access to such therapies as were entering the market in developing countries that had extremely limited resources for expenditure on healthcare.
In the years following the adoption of the original Guidelines, a number of important developments occurred. They demanded reconsideration of the foregoing language of Guideline 6. These developments included the arrival of ARVs; the realisation of their significant impact on the well-being and life expectancy of the patients who receive them; the effect of ARVs (especially Nevarapine) in the significant reduction of mother to child transmission at relatively little cost; the widespread availability of ARVs in developed countries but the virtual unavailability of these therapies in countries of the developing world; and the steps taken at Doha in November 2001, at the Ministerial Conference of the World Trade Organisation, to declare that the Agreement on Trade-Related Aspects of Intellectual Property Rights (TRIPs) should be interpreted to support public health and to allow for patents to be qualified if required to respond to public health emergencies such as the AIDS epidemic. [27]
In consequence of these developments, a new consultation took place in Geneva to revise Guideline 6. I also chaired the new consultation which occurred in July 2002. At the forefront of the consideration by the Expert Group were a number of key documents of the UN. These included the Declaration of Commitment on HIV/AIDS of the General Assembly of the UN, [28] the Millennium Development Goals declared by world leaders at the UN in September 2000, [29] the resolutions of the UN Commission on Human Rights on the Right to the Highest Attainable Health Standard, [30] on Access to Medication [31] and General Comment 14 of the UN Committee on Economic, Social and Cultural Rights. [32]
In consequence of the fresh deliberations of the Expert Group, a revised Guideline 6 was adopted in 2001, in the following terms:
States should enact legislation to provide for the regulation of HIV-related goods, services and information, so as to ensure widespread availability of quality prevention measures and services, adequate HIV prevention and care information and safe and effective medication at an affordable price.
States should also take measures necessary to ensure for all persons, on a sustained and equal basis, the availability and accessibility of quality goods, services and information for HIV/AIDS prevention, treatment, care and support, including antiretroviral and other safe and effective medicines, diagnostics and related technologies for prevention, curative and palliative care of HIV/AIDS and related opportunistic infections and conditions.
States should take such measures at both the domestic and international levels, with particular attention to vulnerable individuals and populations.
Coinciding with this development of principle, WHO and UNAIDS adopted a global initiative to provide antiretroviral therapy to three million people with HIV/AIDS in developing countries by the end of 2005. This strategy has become known as the 3 x 5 Strategy. [33]
Dr Lee, the Director-General of WHO, declared: [34]
Lack of access to antiretroviral treatment is a global health emergency . . . To deliver antiretroviral treatment to the millions who need it, we must change the way we think and change the way we act.
It is at this point that the second AIDS paradox enters for consideration. In advance of the 3 x 5 Strategy, scientific commentators on the 'rights-based approach' began to question the effectiveness of this approach, at least in the circumstances of developing countries and specifically the countries of Africa. One of the key proponents of the need for rethinking has been Dr Kevin M de Cock of the United States Centers for Disease Control and Prevention based in Nairobi, Kenya. Writing in The Lancet, [35] Dr De Cock and his colleagues suggested that it was time to return to what was, in effect, a more conventional public health strategy to combat HIV/AIDS, with much less emphasis on consent and information for the individual. In effect, the message of Dr De Cock and his co-writers has been that communitarian rather than individual approaches should dominate the response to HIV/AIDS. Thus it was put: [36]
Prevention and care in Africa need a serostatus-based approach . . . aimed at universal voluntary knowledge of serostatus, simplified clinical testing, and prevention of discrimination. Defining different categories of testing, consent, and counselling is necessary. International agencies should re-assess their HIV testing policies on the basis of public health needs and targets, and the declared global emergency relating to treatment. Of three possible positions, staying silent will abdicate leadership, and endorsing traditional practice will reinforce barriers to prevention and care; only strong guidance to promote and facilitate HIV testing will allow urgently-needed expansion of treatment and prevention services.
Was this an attempt to return to the siren calls for widespread mandatory testing, initially common in the United States, that was knocked on the head as futile and ineffective in the early days of the HIV/AIDS pandemic?
Was it a Trojan horse for the current moralistic views promoted, most especially in the United States, designed to restore traditional public health control and to identify those morally responsible for spreading a dangerous virus? Would widespread mandatory testing actually be followed up by the provision of ARVs to poor people in Kenya and other countries of Africa and the wider developing world? If not, was such widespread testing simply a diversion of scarce resources to combat this epidemic without the sure promise of any benefit for those tested? Or was Dr De Cock's intervention a serious scientific one based upon the changing features of the epidemic, the availability of affordable ARVs in the form of generic drugs and the manifest need to conduct more HIV tests in order to identify those who could benefit from the ARVs if they could be made available in mass quantity?
For the past two years I have been serving with a distinguished group of scientists, ethicists, lawyers and public health experts on a Reference Panel established by UNAIDS to examine questions of HIV/AIDS and human rights. The questions presented by the views of Dr De Cock have been considered by the Reference Panel. The consideration has been undertaken in the light of the Guidelines on HIV/AIDS and Human Rights, including the revised Guideline 6, the UN Resolutions, and the new WHO/UNAIDS 3 x 5 Strategy.
Clearly, the Panel has appreciated that we are in a new international situation that demands new thinking and a willingness, if necessary, to reconsider past approaches. We now have the ARVs. A new inexpensive and generally accurate saliva test for the presence of HIV has been developed that facilitates HIV testing on a mass scale. The development of generic drugs, available under licence to countries in the developing world to reduce significantly the cost of ARVs and other treatments, together with national contributions and the establishment of the Global Fund [37] to support the provision of therapies in developing countries, make possible what was hitherto thought completely unaffordable. Shame and stigma abound as an impediment to people living with HIV coming forward to undergo tests and to receive therapies. At least, in South Africa, many do not come forward until they are seriously unwell and therefore less amenable to treatment by the available therapies. It is in these circumstances that consideration must be given to whether the past strategies of pre-test voluntary counselling and testing need to be modified or qualified in various ways in order effectively to 'scale up' the testing so as to bridge the reticence and impediments and to get the ARVs quickly to those who need them. Would such a change result in scaling up and effective treatment?
There can be no doubt that the inequalities in the availability of ARVs throughout the world are serious, continuing and a grave affront to human rights and fundamental freedoms. A figure sets out the coverage of adults in developing countries with antiretroviral therapy by reference to the WHO regions in 2003:
Figure 2
Access to ARVs
|
Region |
Number of People |
Estimated |
Coverage |
|
|
on Treatment |
Need |
% |
|
Africa |
100 000 |
4 400 000 |
2 |
|
Americas |
210 000 |
250 000 |
84 |
|
Europe (Eastern Europe, |
15 000 |
80 000 |
19 |
|
Central Asia) |
|
|
|
|
Eastern Mediterranean |
5 000 |
100 000 |
5 |
|
South-East Asia |
60 000 |
900 000 |
7 |
|
Western Pacific |
10 000 |
170 000 |
6 |
|
WHO ALL |
400 000 |
5 900 000 |
7 |
|
REGIONS |
|
|
|
What is the lesson from these statistics? Is it that we should redouble efforts to secure coverage of those who would benefit from ARVs in proper compliance with human right protecting principles of pre-test voluntary and informed consent, as is generally observed in the developed world? Or is it that the special needs of the developing countries, notably in Africa, are so large, so urgent, so intractable and so bedevilled by stigma and discrimination, that systems of routine testing must be introduced with less emphasis upon notions of individual patient prior consent? Is this the only practical way to overcome stigma, fear and apathy? Would it do so in practice? Is it undesirable because it involves a misuse of the human rights of highly vulnerable and poor people who do not need to have such affronts piled upon their serious health status? [38]
The UNAIDS Panel on HIV/AIDS and Human Rights has emphasised that, in the context of the AIDS epidemic, the content of human rights principles is not inflexible. There is an equation that reflects the necessary adjustment of the content of human rights to the circumstances of the epidemic and its proper management. [39] The Panel supports the 3 x 5 initiative. It supports necessary 'scaling up' of HIV testing that is the prerequisite to providing ARVs to those who are infected. However, to be effective, the 'scaling up' must occur in circumstances that are sensitive to the fundamental considerations that are at stake. These include the way the tests are conducted; the access to sustainable treatment and care to which they must lead; the sufficiency of the existing healthcare infrastructure to respond; the provision of laws and policies to protect people against related stigma and discrimination; and the legal and policy context in which the 'scaling up' occurs.
The ethical dilemmas presented by the reality on the ground in Africa, as this epidemic enters its third decade, demand flexibility of approach and a greatly heightened sense of urgency. Clearly, the current predicament is intolerable. Urgent measures are essential. This is one of the largest and most urgent problems for human rights in Africa, indeed the world. As with most human rights questions, there are no easy solutions. But the beginning of wisdom is an appreciation that this epidemic presents acute human rights dilemmas. They derive from the huge challenge to the right to live and the equal challenge, faced by millions, because of the lack of access to basic healthcare essential to human dignity and life.
4. A turning point?
In his address as President of South Africa to the first Joint Sitting of the Third Democratic Parliament in Cape Town on 21 May 2004, President Thabo Mbeki detailed the enormous range of challenges that South Africa faces and the programmes of his government designed to address them. In the midst of so many challenges of the post-apartheid society, HIV/AIDS attracts a paragraph in a speech of 13 pages. But it was one with a clear commitment: [40]
We have already started with the implementation of our Comprehensive Plan on HIV and AIDS. 113 health facilities will be fully operational by March 2005 and 53 000 will be on treatment by that time. At the same time, more impetus will be given to the Khomanani Social Mobilisation Campaign as we intensify home-based care.
It must be hoped that the failure to specify that the 'treatments' promised will include ARVs is inconsequential and that a full range of modern therapies will be provided to South Africans, including ARVs. If South Africa, with its developed medical and hospital infrastructure and high professional standards, can give a lead to Africa in this respect, a great blow will be struck for basic human rights in an area where they have been neglected and are greatly at risk.
The political leaders of the African continent, indeed of the world, must be rendered accountable. So must the UN and its agencies. We have passed the point of cautious plodding. Clearly, the time has come for brave and strong action. But what does strong action require?
If I was in any doubt of the need, the doubt was dispelled when I visited the Chris Hani Baragwanath/Kalafong Hospital on the edge of Soweto during my visit to South Africa. The waiting rooms were full with anxious mothers and sickly children. Very few men were to be seen waiting on the benches. African men, it seems, do not easily acknowledge their vulnerability to HIV, until the end. The lists for admission to the Wellness Clinic at the hospital are overfull and now closed. No new patients can be added to those lists. Pamphlets tell the patients how they can inform others that they are HIV positive. They tell them of the therapies that are available. But are they available to all? Or are they only available to the most 'innocent' of the 'victims'? Is this why men do not come forward because they are seen as 'guilty' and excluded from the treatment regimes? In a continent of so many health care and other problems, is HIV/AIDS just the latest grave health problem that must be borne with fortitude in lives that are rarely far from suffering?
In an earlier address at the National Judicial Symposium, President Mbeki, [41] an economist, drew an analogy between the transformation of South African society and the change of a business. He quoted Francis Goillart and James Kelly [42] as saying:
Transformation . . . is the time when [you] leave the secure walls of the castle and step into unexplored territory. Though the dynamics of success may eventually lead to elation, it is not much fun in the initial stages. There are walls of reluctance and denial to break through, old values to discard, and new ones to assimilate. And that is usually painful, because the ramparts are thick, and they are made of human emotions and prejudices.
President Mbeki told the assembled judges of South Africa of the need, in the law, to break down the walls of reluctance, to discard old values, to assimilate new values and to establish mastery over human emotions and prejudices. He urged them to take the road that Chief Justice John Marshall of revolutionary America had chosen 200 years earlier so that the 'better angels of our nature' would prevail.
That is what is needed in South Africa, in Africa and the world as we face the third decade of HIV/AIDS. We are still in the initial stages. There is no fun whatever in the struggle. The walls of reluctance and denial so often seem impenetrable. The old values that impede the struggle (some of them lately reinforced) remain. The new values are yet to be accepted. And meanwhile, in the hospital wards, in the villages, in the fields, indeed everywhere, people are sick, gravely ill and dying. We must help them.
That is what human rights is about: human dignity and justice. Nothing less will do. How we go about attaining human rights is also important. We must maintain the struggle to prevent the infection of new generations. We must not write off the millions who are already infected with HIV and can now be helped by therapies and by behaviour modification. And in responding to the dilemmas of AIDS we must be fresh of mind, constantly alert to the paradoxes of AIDS and the cries of the vulnerable. Neglect is contemptible. Moralising is counter- productive. Men, women and children are in need. They have human rights. They have rights to justice. We all have human duties to respond.
[1] 'R Riddick 'State of denial: Finding meaning in South Africa's AIDS crisis' (2003-4) 24 Conscience 35; M Modise et al 'Stopping AIDS in Africa' (2004) Melbourne University Magazine 21.
[2] It is estimated that at least 4,5-5 million South Africans are infected with HIV. See University of Pretoria, Centre for the Study of AIDS HIV/AIDS and human rights in South Africa (2004) 6.
[3] HW Haverkos & JA Dougherty (eds) Health hazards of nitrate inhalants (1988). See also J Lauritsen & H Wilson Death rush: Poppers and AIDS (1986).
[4] P Piot et al 'Acquired Immunodeficiency Syndrome in a heterosexual population in Zaire' (1984) 2 The Lancet 65-69.
[5] N Clumeck et al 'Acquired Immune Deficiency Syndrome in black Africans' (1983) 1 The Lancet 642.
[6] MD Kirby 'AIDS legislation — Turning up the heat?' (1986) 60 Australian Law Journal 324.
[7] MD Kirby 'The new AIDS virus — Ineffective and unjust laws' unpublished paper for the International Symposium on AIDS, Paris, 23 October 1987, reprinted in Washington Post 2 February 1988 12.
[8] WM McNeill Plagues and peoples (1976); PH Curson Times of crisis: Epidemics in Sydney, 1788-1900 (1985).
[9] T Mangold 'The plague mentality makes victims of us all' The Listener 2 July 1987 546.
[10] MD Kirby 'The ten paradoxes of AIDS — Summing up the First International Conference on the Global Impact of AIDS', London, 8-10 March 1988 in AF Fleming et al (eds) The global impact of AIDS (1988) 397.
[11] J Mann 'Health and human rights: If not now, when?' (1997) 2 Health and Human Rights 118.
[12] W Bowtell 'HIV/AIDS: Present at the creation' unpublished paper to the HIV/AIDS, Hepatitis C and Related Diseases Social Research Conference, Sydney, 18 May 2004. See also P Sendziuk Learning to trust: Australian responses to AIDS (2004) and N Blewett 'AIDS in Australia: The primitive years' Commissioned Paper Series, Australian Health Policy Institute (2003/07).
[13] Human Rights (Sexual Conduct) Act 1994.
[14] Sec 124 Criminal Code 1924 (Tas).
[15] Communication 488/92, Toonen v Australia, CCPR/C/50/D/488/92, 31 March 1994, reproduced in HJ Steiner & P Alston International human rights in context (1996) 545-548.
[16] J Godwin et al Australian HIV/AIDS legal guide (1993) ch 8 'Sex Industry' 242.
[17] n 16 above, ch 4 'Anti-discrimination and equal opportunity', 87. See also IW v City of Perth (1997) 191 CLR 1 and X v The Commonwealth (1999) 200 CLR 177.
[18] Reproduced in MD Kirby 'Foreword to LO Gostin' The AIDS pandemic: Complacency, injustice and unfulfilled expectations (2004) xi xv.
[19] 'AIDS out of control' Sydney Star Observer 15 July 2004 1.
[20] As above.
[21] As above.
[22] H Burkhalter 'The politics of AIDS: Engaging conservative activists' (2004) 83 Foreign Affairs 8.
[23] Art 6 CCPR. In its General Comment, the UN Human Rights Committee describes the right to life as a 'supreme right' and a right 'basic to all human rights'. See General Comment No 14 reproduced in (1994) 1 International Human Rights Reports 15-16, confirming the earlier General Comment No 6 reproduced in (1994) 1 International Human Rights Reports 4-5. Municipal courts have frequently ranked the right of an individual to life as 'the most fundamental of all human rights'. See Bugdaycay v Secretary of State for the Home Department [1987] AC 514 at 531 per Lord Bridge of Harwich cited with approval in R v Lord Saville of Newdigate & Others; Ex parte A [2000] 1 WLR 1855.
[24] Art 12 International Covenant on Economic, Social and Cultural Rights. The UN Human Rights Committee has recognised a connection between the right to life and a state's obligation to provide medical care. In its General Comment on the right to life, the Committee urged state parties to take all possible measures to reduce infant mortality and to increase life expectancy. See UN Human Rights Committee, General Comment No 6 (n 23 above) para 5. See also Soobramoney v Minister of Health, KwaZulu-Natal 1997 12 BCLR 1696 (CC); 1998 1 SA 765 (CC).
[25] Office of the High Commissioner for Human Rights and UNAIDS HIV/AIDS and human rights — International guidelines (1998) (HR/pub/98/1) (reprinted 2001).
[26] Office of the High Commissioner for Human Rights and UNAIDS, HIV/AIDS and human rights — International guidelines — Revised Guideline 6 — Access to prevention, treatment, care and support (Geneva, July 2002) (UNAIDS/02 49E) 21-22.
[27] Statement by Dr Peter Piot, Executive Director, UNAIDS and Mary Robinson, High Commissioner for Human Rights in Revised guideline 6 (2002) 6.
[28] UN General Assembly Declaration of Commitment on HIV/AIDS ('Global crisis — Global action') Resolution A/RES/S-26/2 (27 June 2001).
[29] UN General Assembly United Nations Millennium Declaration Resolution 55/2 A/RES/55/2 (8 September 2000).
[30] E/CN 4/RES/2002/31.
[31] E/CN 4/RES/2001/33, E/CN.4/RES/2002/32.
[32] General Comment No 14: The right to the highest attainable standard of health, adopted 11 May 2000; E/C 12 2000/4.
[33] World Health Organisation and UNAIDS Treating 3 million by 2005 — Making it happen — The WHO strategy (2003).
[34] n 33 above, 1.
[35] KM de Cock et al 'A serostatus-based approach to HIV/AIDS prevention and care in Africa' (2003) 362 The Lancet 1847; KM de Cock et al 'Shadow on the continent: Public health and HIV/AIDS in Africa in the 21st century' (2002) 360 The Lancet 67.
[36] The Lancet (2003) (n 35 above) 1848.
[37] The Global Fund to Fight AIDS, Tuberculosis and Malaria (Executive Director, Dr Richard Feachem). There are also bilateral programmes such as the US Presidential Emergency Plan for AIDS Relief (USA) and private programmes, such as those initiated by the Gates Foundation (USA).
[38] For a recent South African case involving unconsensual testing of a domestic worker for HIV and Hepatitis B and a claim under the Labour Relations Act 1995 (South Africa) of unfair dismissal under s 187(1)(f), see AIDS Law Project 'Domestic workers and HIV/AIDS' http://www.alp.org.za/view/php?file-/kyr/20040608_DomWork.xml (accessed 31 July 2004).
[39] S Gruskin & B Loff 'Do human rights have a role in public health work?' (2002) 360 The Lancet 1880.
[40] T Mbeki 'Address of the President of South Africa to the First Joint Sitting of the Third Democratic Parliament' 21 May 2004 8.
[41] T Mbeki 'Address to the Judicial Symposium' (2003) 120 South African Law Journal 652.
[42] n 41 above, 657, citing F Gouillart & J Kelly Transforming the organisation (1995).

